The Crescer project is implemented by a consortium consisting of five partners; two Angolan institutions (Universidade Mandume Ya Ndemufayo and Fundo de Apoio Social) and three from Spain: the Hospital Universitari Vall d’Hebron Research Institute (consortium’s coordinator), the Instituto de Salud Carlos III and Action Against Hunger Spain. The European Union funds it.
Study design
The study is conceived as a community trial, controlled, open, non-inferiority, randomized by clusters, with three intervention arms grouped by blocks (communes) in parallel groups, in two provinces of Southern Angola, Huíla and Cunene. The cluster allocation ratio is 1:1:1.
The study is prospective, pregnant women will be recruited and followed along their newborns until the children turn 2 years old.
Study setting
The MuCCUA trial is set in two provinces of Southern Angola: Huila and Cunene. The most recent official data on malnutrition estimates that the prevalence ofstunting in selected areas of Huila and Cunene provinces is 50% and 37% respectively, and the prevalence of acute malnutrition around 11% in both provinces for children under five years of age. In addition, the prevalence of stunting in children below 2 years of age raises to 51.8% in Huila and to 44.6% in Cunene [19].
The trial is carried out in these two provinces (admin 1 level). Two municipalities (admin 2 level) per province were selected with one commune (admin 3 level) per municipality (total two communes per province); the commune of Libongue (Chicomba municipality) and the commune of Jamba (municipality of Jamba) in the province of Huíla. The commune of Otchinjau (municipality of Cahama) and the commune of Mupa (municipality of Cuvelai) in Cunene province. See Fig. 1.
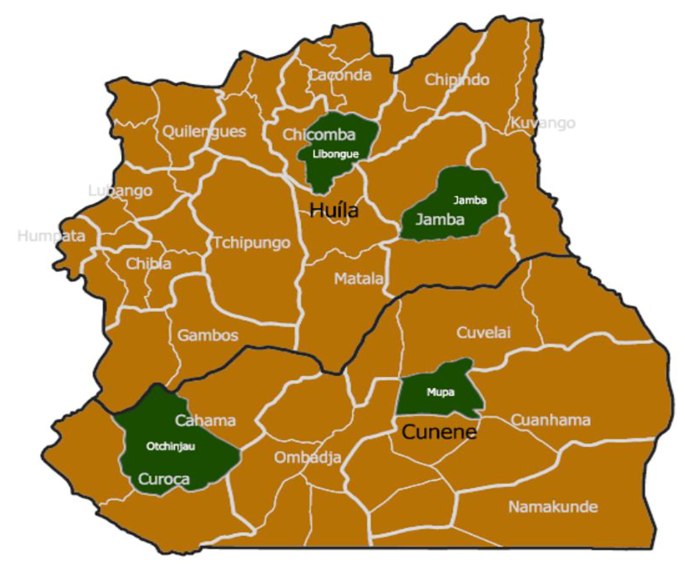
Study communes (green) within Huila and Cunene provinces
The interventions
The standard of care intervention is provided at cluster level, the cash transfer, and nutrition supplements interventions at the individual level.
Standard of care arm (SoC arm)
The new national policy for community development of the Ministry of Territorial Administration of the Republic of Angola foresees the implementation of a standard of care program to be delivered by a new figure, the ADECOS (Agentes de Desenvolvimento Comunitário e Sanitário) through the Institute of Local Development-Social Support Fund (FAS), included in the Health Community Workers classification. The ADECOS emerged as one of the strategies with more potential to address cost-effectively the scarcity of health human resources in remote areas, as they should be able to provide culturally competent services to improve accessibility to primary health care and community awareness in water, hygiene and sanitation (WASH), nutrition, and health related good practices.
This policy is in different implementation phases across the country by the Government of Angola, but the Southern provinces have not yet started its implementation at the health care level. Thus, in the study areas of the provinces of Huila and Cunene, the Crescer project financed its implementation through the FAS, one of the partners of the Crescer consortium.
The activities to be developed by the ADECOS can be summarized in two types:
Health promotion activities: including bi weekly home visits and quarterly community activities to promote adequate management of acute malnutrition and promotion of appropriate caring and feeding practices with special emphasis on breastfeeding, and sensitization sessions to promote adequate hygiene and sanitation.
Preventive pharmacological activities: these are conducted quarterly and include malaria prophylaxis in pregnant women, deworming in pregnant women and children between 12 and 59 months, and vitamin A supplementation in children 6 to 24 months of age.
The standard of care includes in its package many of the evidence-based interventions to tackle malnutrition identified in the 2013 Lancet Series [7] and may have an important impact on stunting in a population as deprived as the one in our study, although up to date, and as far as we know, there is no evidence on this effect.
Standard of care + nutritional supplementation arm (SoC + NS arm)
Communities allocated to this arm receive the Standard of care intervention plus a nutritional supplementation to families with at least one pregnant woman. Nutritional supplementation consists of a daily intake of small quantity lipid based nutrients supplement (SQ-LNS) for the pregnant women and their newborn children and a complementary food ration for their families, as described below.
-
Individual ration of SQ-LNS: Nutriset Enov’ Mum™ for pregnant and lactating women until their new-born turns 6 months (1 sachet of 20 grs/day) and Nutriset Enovnutributter ®+ for the newborn children after their 6th month and until the child turns 24 months of age (1 sachet of 20 grs/ day).
-
Complementary family food ration: basket of locally produced staple foods that complement the usual diet (300 Kcal/person/day). The caloric distribution of the basket will be 45% of cereals (corn meal – carbohydrate), 30% of legumes (beans – vegetable protein) and 25% of oil (soybean oil – fat). In addition, 1 kg of iodized salt will be provided.
The individual ratios of SQ-LNS will be distributed to households by the local ADECOS every two weeks, and the family ration by the project distribution team every three months in the central distribution point.
Out of the three interventions assessed, this intervention has the greatest evidence of its effect on stunting. Dewey meta-analysis showed that SQ-LNS provision led to a 12% stunting reduction (relative average) [14]. This arm will be usedas a comparator as it serves the primary purpose of the trial, and it fulfils the criteria of acceptability, feasibility, formidability and relevance required to be a good comparator [20].
Standard of care + cash transfer arm (SoC + CT arm)
Communities allocated to this arm will receive the Standard of care intervention plus an unconditional cash transfer given to families with at least one pregnant woman as describedbelow. The pregnant woman, as the main participant, is defined as the cash transfer recipient.
A total of 13,855 kwanzas per month is delivered to families with four or more members living in the household during the study period, and 10,855 kwanzas per month to families with less than four members living in the household during the period of study. The minimum inter professional salary in Angola at the time being is set at 35,000 kwanzas per month.
The amount is delivered in cash with unconditional format. The cash transfer will be distributed to the recruited women or persons authorized by her every three months in a central point of distribution.
Study participants
The study population are pregnant women over 16 years of age living in the selected clusters, and their newborn children. The target population of the interventions are all the members living in the household where the pregnant woman lives. In the study area, a household oragregado familiar is defined as the group of people, with or without kinship relationships, that usually live together under the same roof, and for at least 6 months (or less than 6 months, but with the intention of staying in the residence for the next 6 months), and share food and/or other vital needs, and their house.
All pregnant women living in the selected cluster can be included in the study, up to a maximum of 40 per cluster.
Sample size
We used the results from the most recent SMART survey [19] to determine the chronic malnutrition prevalences for the sampling computations, assuming an overall stunting prevalente in children under 2 years of 47,5%. We estimate an expected effect of the nutritional supplementation plus standard of care intervention to reduce stunting by 9.8%, and the same (9.8%) for the experimental arms (standard of care alone or standard of care plus cash transfer arms). Although the literature provides lower effects of stunting reduction for SQLNS interventions [14], we have assumed a higher effect due to several factors including that the SQLNS individual supplementation starts during the mothers pregnancy and is continued until the age of 2 years of the child, and is complemented with a food family ratio at household level. Moreover, the three arms involve the implementation of an optimized standard of care at community level that targets many of the underlying causes of malnutrition, enhancing the effects of any individual intervention. Finally, the area of study has suffered an important food crises in the last two years and thus population is at high risk of food insecurity and with increased potential to benefit from the interventions proposed.
We have assumed an intracluster correlation coefficient (ICC) of 0.006 based in the literature [21], and computed the design effect and inflation factor as follows:
Inflation factor = 1 + [(m– 1) x ICC]
where m is the size of the participants to be included in each cluster thus,
Inflation factor = 1 + [(40–1) x 0.006] = 1 + [39×0.006] = 1 + 0.234 = 1.234
The 15% was added as expected follow-up loss rate (estimated based on perinatal mortality, 50.2 per 1000 live births, according to World Bank dataFootnote 1).
The study was conceived as a community trial, controlled, open, non-inferiority, randomized by clusters.
Thus, it’s necessary to recruit 12 clusters per each arm with 40 subjects per cluster to achieve 80% power to detect a difference of 0 when the non-inferiority difference is 0.098. The proportion in the experimental groups (SoC alone or SoC + CT) is assumed to be 0.475 under the null hypothesis and 0.377 under the alternative hypothesis. The proportion in the comparator group (SOC + SN) is 0.377.
In all cases the statistic test used is the one-sided Likelihood Score Test (Farrington & Manning). The intracluster correlation is 0.006, and the significance level of the test is 0.025.
In Table 1 and in Fig. 2 we show the distribution of the clusters.
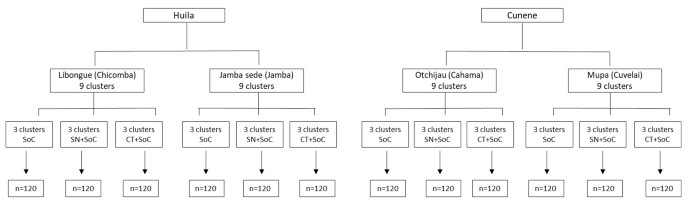
Clusters allocation and expected sample size
Study clusters
Study clusters refer to villages or neighbourhoods (both referred in this text as communities interchangeably). Being that we need to recruit 40 pregnant women per cluster, we calculated the necessary population size of the cluster with the 3,72% pregnancy prevalence provided by local health authoritiesFootnote 2 and that calculation resulted in a cluster size of around 1075 people.
We worked with local authorities to identify the villages and neighbourhoods that fulfilled the inclusion criteria. These were listed, along with their estimated populations, and were geographically located in maps elaborated by the project. We then elaborated a list of eligible clusters by: (a) identifying as clusters those communities with a population size around 1075, (b) subdividing larger villages and neighbourhoods into smaller population units of around 1075 people and identifying them as clusters and (c) grouping small and proximate villages to compose additional clusters of the required 1075 population size.
The study design was randomized by clusters with the three intervention arms grouped by communes thus; we had separate clusters’ lists for the communes and in each of the communes we displayed a public ceremony with local administration and community leaders. The names of all potential clusters within the commune were written in folded pieces of paper and placed in a lottery ballot, from which they were taken randomly to guarantee concealment.
Once the clusters to participate in the study were selected, we proceed with the recruitment and random allocation of clusters to the different arms of the study.
Recruitment and random allocation
The recruitment of the clusters was done by sensitisation sessions with the local authorities to whom the study design and planned interventions were explained in detail.
The local authorities (named Sobas and Seculos in Angola) had to sign an informed consent to allow for the participation of their communities in the study, before knowing to which arm their community was going to be allocated.
After signing the informed consent, a community leader representing the cluster had to take a slip of folded paper from a lottery ballot box where each folded paper contained the name of one intervention arm. The cluster of the community leader picking up the paper was then allocated to the intervention arm written in the paper. This way allocation concealment was guaranteed. In each commune, three clusters were allocated to each of the intervention arms.
For the recruitment of participants, the week before the first field visit, local ADECOS conduct an active search to identify the pregnant women in the community. They visit the households to inform and sensitise all members of the family as well as pregnant women about the study to take place and the need of their participation in the upcoming survey visit. If ADECOS feel reluctance or uneasiness in the household about being part of the study, they approach the community leader and request his mediation to sensitise the family to the objectives of thestudy.
The allocation of participants was done by complete enumeration. Up to 40 women living in the selected cluster were recruited by order of identification by the ADECOS in the previous weeks, and receive the intervention allocated to their cluster. Women were requested informed consent to participate in the study after informing them about the study overall and about the arm of the study they had been allocated to.
Eligibility criteria
Inclusion criteria
For municipalities.
-
Be considered as one of the municipalities prioritized by the FRESAN program;
-
Have a multidimensional poverty level of 4 or 5 according to the Angola National Statistical Institute classification;
-
Acceptance by local and traditional authorities.
For communes.
For communities [Villages (aldeias) and neighbourhoods (bairros)]
-
Do not have other interventions of monetary or nutritional transfers (nutrition-specific or nutrition-sensitive) in place or forecasted at the time of the inclusion in this study;
-
Acceptance by local authorities through the informed consent form signed by the community leader;
-
Place accessible by a 4 × 4 vehicle (especially during the rainy season);
-
Have a reference health post with reference health personnel.
For participants.
-
Women 16 years and above;
-
Pregnancy confirmed by pregnancy test;
-
Acceptance to participate in the study through the free and informed oral consent form confirmed and signed by a research investigator;
-
Live newborns of the participant pregnant women;
Exclusion criteria
For participants.
-
Women 16 years of age or above, pregnant, who do not belong to pre-selected neighbourhoods/villages;
-
Women who don´t live in the household in a regularly manner;
-
Women who have planned to travel or move out of the neighbourhood within the follow-up period of the study;
-
Women who express the impossibility of attending the follow-up visits;
-
Women with a history of alcohol abuse (considered as intake of > 3 drinks on any day or > 7 drinks per week);
-
Any condition that may affect the intervention/follow-up compliance (at the discretion of the investigator);
-
Pregnant women with acute malnutrition (arm circumference < 21 cm).
Outcome measures
The outcomes are measured at individual level, but analysis and interpretation will be made only at cluster level.
Primary outcome
Secondary outcomes
-
Child mortality rate at 3, 6, 12, 18 and 24 months of age.
-
Proportion of neonatal low birth weight, and low birth weight for gestational age.
-
Proportion of children with anaemia (Hb < 12 g/dL) at 6, 12, 18 and 24 months of age.
-
Cumulative incidence of morbidity (mainly malaria, diarrhoea and pneumonia) in children below 2 years of age at 3, 6, 12, 18, and 24 months of age.
-
Primary household caregiver’s knowledge, attitudes and practices related to perinatal and children’s caring practices including breastfeeding and hygiene and sanitation at baseline and endline.
-
Women and children minimum dietary diversity at baseline and endline, and at 3, 6, 12, 18 and 24 months of age of the participant child.
Measurements
Data collection tools
Questionnaires
At baseline and end line, we use self-elaborated questionnaires to collect general information of the household, as well as specific information of the head of the household, the primary household caregiver and the participant pregnant women. Sections in these questionnaires include: sociodemographic data, household assets, food security, knowledge, attitudes and practices related to children’s caring practices as well as hygiene, and sanitation, women’s empowerment, dietary diversity at household, women and children’s level, perinatal care and pregnant women’s morbidity and mental health.
For the food security section we used the FAO standardized survey modules on household dietary diversity score [22] and on the food insecurity experience access scale (FIES) survey module [23]. To measure women’s dietary diversity we used the Minimum Dietary Diversity for Women questionnaire [24] adapted to Angola by the Global Diet Quality ProjectFootnote 3, and to assess children’s dietary practices we used the standardized survey modules provided by the World Health Organization and UNICEF [25].
In the follow up visits, data will be collected from study participants with specific self-elaborated questionnaires (mothers and children’s questionnaires).
Original questionnaires are in Portuguese and translation to local languages was conducted during the training with enumerators.
The questionnaires are in digital format, designed with the Ennov Clinical Software, and data is collected with the application Ennov Clinical through smart devices run on apple-based platforms. Data is sent to the data management centre every few days upon internet coverage availability.
Anthropometry
Arm circumference is measured in pregnant women and children using standard MUAC bracelets.
During the survey, women identified with a MUAC below 210 mm are referred to the nearest health facility for standard treatment. Children identified with a MUAC < 125 mm are referred to the nearest out-patient therapeutic centre.
Body weight (kg) and height (cm) are measured in children. Weights are measured using the ADE M321600 electronic floor scale with mother and child weighing function.
Height is measured in children (standing or recumbent) using a wooden board suitable for measuring the length of infants and the height of children up to 160 cm.
Biochemical measures
Women identified as pregnant in the community are tested with the DIAGNOS© hCG one-step pregnancy tests to confirm their pregnancy status. If a negative result is obtained the test is repeated, and if a negative result is again obtained, the woman is referred to the health centre for follow up and she is excluded from the study.
Haemoglobin is measured using the Very-Q RED haemoglobin monitoring system (0.1 g/dl accuracy) in the participant women during visits where she is pregnant and in participant newborn children at age 6 months, 12 months, 18 months and 24 months. If any participant is identified with an Hb < 5 g/dl is referred to the nearest public health facility.
Malaria infection is measured with Abbot Malaria Ag P.f/Pan rapid test in children at 6, 12, 18 and 24 months of age. Children identified with a positive result are referred to the nearest health facility for standard treatment.
Physical examination
Nursing and medical students perform a physical examination of participants and follow a standardized procedure of health care indications and referral to health facilities for any danger sign observed, including an Hb < 7 g /dL with symptoms.
Data collection team
There are 12 teams of enumerators supervised by three research investigators and three field supervisors. Each team is composed by one medical or nursing student and one ADECOS and both received previous training for conducting the interviews and entering the data.
A total of 54 ADECOS (out of the 214 recruited by Crescer) participate in the data collection and are trained in survey procedures. The training for data collection was done to pairs of students and ADECOS as they have different roles to play during the survey implementation. The students are in charge of asking and recording the responses in the tablet, as well as taking the measurements and doing the physical examination. The ADECOS are responsible of introducing the team to the families and acting as translators during the interviews, as well as supporting with the measurements when required.
Enumerators and supervisors were also trained in anthropometric and biochemical measurements according to international recommendations, as well as in the standard operational procedures elaborated for the data collection activities.
Pilot studies were conducted as part of the field work training and to test the tools in both Huila and Cunene provinces.
Data collection timeline
The recruitment and baseline survey has started in 10 October 2022 and will continue until March 2023, thus recruitment is ongoing at the time of submission of this protocol for publication. The research team makes field visits every 3 months in order to collect baseline measurements on all study households (household questionnaire) and participants (pregnant women), and follow up data on participants (mother and child questionnaires) until the newborn child turns 2 years of age (end line survey). Thus, the end line surveys will be conducted at different times, depending on the date and the gestational age of the women at the time of recruitment, with dates for end line surveys ranging between November 2024 andFebruary 2025.
The SQ-LNS Supplementation and the unconditional cash transfers are implemented during the quarterly visits. See Table 2.
Depending on the gestational age of the pregnant women and the age of the child at the time of the visit different data will be collected. Women will complete one or two questionnaires during pregnancy (around 6th month of pregnancy and/or around 9th month of pregnancy). In addition, once the children are born, all women and newborn children included in the study will be surveyed (mother and child questionnaires) at 3 months, 6 months, 12 months, 18 months and 24 months of age of the children with a precision range of 45 days. Outcomes to be collected at those time points are detailed in Table 3.
Planned statistical methods
The analysis will be done only at cluster level. Descriptive analyses will be carried out in all independent variables at cluster level to characterize groups at baseline and identify potential differences between them.
Categorical variables will be presented as frequencies and percentages and continuous variables as medians (interquartile range) or means (standard deviation) according to data distribution.
Distribution normality will be checked by means of histograms and the Kolmogorov-Smirnov test.
The chi-square test or Fisher’s exact test will be performed to compare frequencies between categorical variables and the Mann-Whitney test or Student’s t-test will be used to compare continuous variables.
For the analysis of effectiveness, the comparison of the proportion of participants with stunting between the clusters will be performed through generalized linear models with log-link and binomial distribution. We will estimate the value of the difference between the experimental interventions (SoC, SoC + CT arms) and the comparator intervention (SoC + NS, arm).
We will do the analyses in two study populations. The one defined per intention to treat (ITT), comprises all randomized participants including those that did not fulfil the inclusion criteria but were randomized, those with an early withdrawal before starting the interventions and those facing major protocol deviations, all of which are considered treatment failures. The other one, obtained per protocol (PP), is the subset of participants belonging to the ITT who do not deviate from the protocol. Thus, it excludes participants facing any deviation from the protocol (do not comply with the instructions of the interventions or interrupt or permanently modify the proposed scheme).
Significance will be set at p < 0.05 level.