Based on interviews with PGY participants about learning discharge planning after completing the curriculum and performing actual cases, the following findings emerged from this study. We first discussed the elements of activity theories, then indicated the four contradictions, and found four PGY’s improvements in the end. We describe each theme below along with sample supporting quotes in Tables 1 and 2.
The elements of CHAT
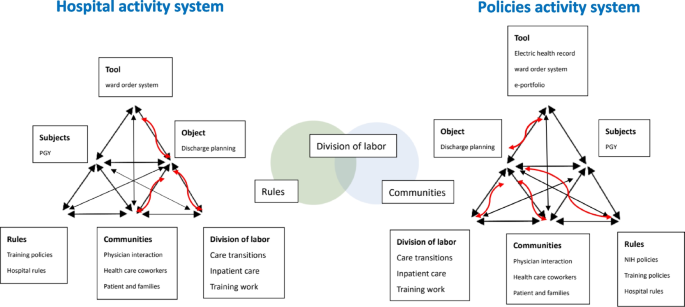
In Fig. 2, this study discusses the elements of CHAT, including communities: disagreements between communities or communication with caregivers; division of labor: daily distribution of work, occasional inability to focus on stable patients being discharged; rules: unable to provide comprehensive patient care due to subspecialty training; and tools: additional time spent following up with patients by phone and completing electronic team medical records.
Systemic contradictions as sources of discharge planning training for PGY
Furthermore, we can find that division of daily work can be positively integrated by using the rules of the national policy and communities of team members (in the middle of Fig. 2).
Communities: differences of opinion across communities
The primary supervisor is the attending physician, who is also the primary decision maker for any disposition or treatment for a patient. Thus, the attitude of the attending physician has a major impact on PGY participants. Conflicts may also arise, but PGY participants respect their teachers and keep these doubts and conflicts to themselves. These problems gradually emerged during the implementation of discharge planning. Since it is a national and hospital policy, physicians tend to implement it and communicate with each other.
S1 Communities: communication with caregivers.
In medical care, “total care” unconsciously deprives patients and their families of the opportunity to learn how to care, causing patients to depend on hospitals. In addition to the guidance by medical staff, the patient’s self-care and the level of commitment of the family are also important in the follow-up care, which requires two-way communication. This explains why the attitude of the patient and the family are also important.
Division of labor: daily distribution of work, sometimes being unable to focus on stable patients to be discharged
The main reason discharge planning is difficult to implement in clinical practice is the field of physician training. Although discharge planning is important, the residents only care about hospitalized patients as the patients to be discharged are typically in stable condition. As a result, it is only natural that the priorities of daily work shift, as in other countries and professions. If the curriculum teaches PGY physicians why discharge planning is necessary and their role in it, it strengthens their self-identification. It takes less time, but improves the quality of care at discharge.
Rules: being unable to provide comprehensive patient care because of subspecialty training
Discontinuity of patient care caused by subspecialty training is a difficulty encountered in today’s medical education. Greysen and colleagues also found PGYs particularly focused on events occurring in the hospital and described follow-up care as beyond their routine care [4]. As learning and care takes place in the hospital, communication with subsequent caregivers is also a major challenge when the patient is discharged.
Tools: additional time required to follow up with patients by phone and complete electronic team medical records
While discharge planning improves the quality of patient care and increases the resident’s ability to discharge plan, it also increases physician workload and causes discomfort for some physicians. While telephone follow-up allows residents to keep track of their patients’ status after discharge, it also requires residents to spend additional time calling patients at specific locations. Sometimes, because of their busy schedules, they forget to keep track of their patients and feel stressed. Therefore, the curriculum can be further adjusted in the future. This is the same situation in all other studies.
Contradiction
There are still some inconsistencies in the teaching and implementation of the discharge planning program for PGY participants that need to be resolved: (1) disagreements across communities or in communication with caregivers; (2) feeling overburdened due to the day-to-day work distribution; sometimes not being able to focus on stable patients being discharged (3) worrying about lack of experience and not providing comprehensive patient care due to subspecialty training; and (4) residents only feeling responsible for hospitalization; they did not like to spend additional time following up with patients by phone and completing electronic team medical records.
Differences of opinion across communities
The program initially targeted PGY participants, but their attending physicians in clinical training have not received the appropriate courses and training. Some still believe that discharge planning should be the sole responsibility of discharge planners. Some PGY participants felt that it was necessary to initiate a discharge planning team for a patient. However, the attending physician disagreed, leading to inconsistencies in the PGY participant’s implementation. If a PGY participant had problems with implementation and asked the attending physician, but did not receive an appropriate response, this could lead to problems and confusion in implementation.
This problem was partially solved by improving electronic physician orders. In the early stages of discharge planning implementation, some physicians are not quite sure whether a patient needs discharge planning or there is no consensus among physicians. If the patient is eligible for follow-up after hospitalization, the physician is advised that discharge planning for that patient should be initiated through the electronic physician order system. Motamedi and colleagues had reviewed that computer-enabled discharge communications appear beneficial and improve timeliness and physicians’ satisfaction [13].
When the physician initiates the team’s plan of care, team members can provide ratings and recommendations through the electronic medical record system. The physician can then discuss and develop the patient’s discharge plan based on the team’s recommendations. Using system reminders and team recommendations, PGY participants could more confidently discuss their patients’ discharge plans with their teachers.
Communication with caregivers
Although the physician–patient relationship has been enhanced, the patient’s primary caregiver may change after discharge, and there are concerns about the subsequent care. A patient’s caregiver while in the hospital could be replaced by someone else after discharge. This can lead to discontinuity in patient follow-up and make PGY participants feel powerless. They believe that even if they give good discharge care instructions, these efforts will be for naught if subsequent implementation fails.
Feeling overburdened
In the PGY training phase, residents have many policy-mandated assignments in addition to their clinical work. At this point, discharge planning seems to be an additional burden on the residents.
Although the physician should make discharge-related medical orders, it is necessary for discharge planning to retain the discussions and records of team meetings. PGY residents must record the minutes of the meetings and keep them in the nursing system. After the patient is discharged from the hospital, the resident must conduct follow-up meetings and record them. Residents in PGY have to make phone calls during office hours to inquire about patients’ discharge status, which puts a lot of stress on them. Inpatient medical issues are complicated, and physicians must prioritize them. Patients who are ready to be discharged or who are discharged in a stable condition are given lower priority.
Worried about the lack of experience
As a direct transition from medical school to residency, PGY participants are the youngest residents in the hospital, and some may still need to adjust. During the training on discharge planning, some participants felt that implementation was somewhat difficult because they lacked experience, for example, insufficient familiarity with other team members’ work. However, some participants felt that learning these things in the PGY phase was consistent with the concept of holistic care. In particular, when the workload of attendings or residents is much heavier and they are not available to do discharge planning, PGY participants need to step in to do it under the guidance of other attendings.
Unable to provide comprehensive patient care because of subspecialty training
Residents are still in the training phase and have to change internal medicine departments every month and see patients at other attending physicians, so they cannot follow the continuing care of their patients. They cannot provide continuous and comprehensive care. However, this problem is present in every residency training system.
Residents only responsible for hospitalization
Some residents feel overworked when caring for their patients and are frustrated with the extra work they have to do during training, as they are caring for patients and also attending classes. They believe that residents only need to take care of the patients in the hospital. Patients will return to the attending physician’s clinic for follow-up after discharge, and residents do not need to know the discharge status of patients. If a patient has a problem after discharge, medical care in Taiwan is convenient, accessible and inexpensive. The patient can return to the hospital and be readmitted for treatment at any time if necessary.
Additional time required to follow up with patients by phone and complete electronic team medical records
Discharge planning requires a team meeting to be documented by the PGY physician and a telephone call to follow up and document the patient’s status at discharge. Initially, telephone follow-ups were documented on paper, but later they were added to the electronic medical record system. However, physicians feel that these records take additional time on top of the daily records.
Participants’ improvement
Participants learn through practice to improve (1) their identification of discharge planning needs, (2) their self-identification within the team, (3) the relationship between team members, and (4) the physician–patient relationship.
Improving identification of discharge planning needs
Interviews revealed that residents understood, based on their training, why discharge planning is necessary, how important it is to patients, and the physician’s role in it. The structure and process developed to remind PGY participants also helped them identify their patients’ needs, improve communication and rapport with team members, contribute ideas, plan post-discharge care during hospitalization, and improve the quality of patient care. Participants felt that their ability to identify patients’ needs at discharge had improved significantly, which was not the case during their internship. They used to do what the physician told them to do without applying their ideas, but after the classes and practical work, they gradually became more aware of the patient’s discharge planning needs.
Improving self-identification
The discharge planning program is sponsored and implemented by Taiwan’s Ministry of Health and Welfare to improve the quality of long-term care. Because it is a government-sponsored program and is included in hospital accreditation, hospitals must implement the program and review and improve the number of patients requiring discharge planning each month. Through the curriculum and hands-on implementation of discharge planning, PGY participants became better integrated into the team, and their self-identification with the physicians’ role in discharge planning was strengthened. This program can create an encouraging atmosphere in hospitals. As team leaders, physicians are more aware of and dedicated to implementing discharge planning.
Self-reporting by physicians also increased significantly. Discharge planners were assumed to be responsible for discharge planning. PGY’s daily care of patients is comprehensive and continuous. Physicians know more about patients’ conditions, functional status, and family and financial situations than discharge planners and nurses working three shifts. Within the hospital, residents are in the best position to understand their patients’ needs, more so than attending physicians. Residents in PGY recognize this and are more self-aware. They no longer rely on discharge planners or attending physicians and can initiate and plan care through the discharge planning team as soon as a patient needs discharge planning.
Improving division of labor and the relationship between team members (know more about other roles although passively)
Okoniewska et al. found that poor communication between care team members can delay patient readiness for discharge and subsequent discharge completion [2].
During the curriculum orientation, other members of the discharge planning team were introduced so that PGY participants knew the job duties of other team members.
PGY participants were required to initiate a discharge planning team meeting with at least two other members, including a pharmacist, dietitian, rehabilitation specialist, psychologist, and discharge planner, to implement the discharge planning process. During the implementation process, participants were able to better understand other roles and responsibilities. When discussing patient discharge needs, participants noted that all roles work together to help patients. Although they were forced to convene a discharge planning team meeting, participants were also more aware of the hospital’s processes and discussed the best options for patient. In the past, physicians often believed that they only needed to contact a discharge planner to discharge their patients. This led to an unclear division of labor in discharge planning and inadequate quality of discharge planning for patients. After the three-month training, the participants became familiar with the team. They were able to actively discuss the needs of hospitalized patients with team members to improve the efficiency of the division of labor.
Improving the physician–patient relationship (discharge follow-up)
Miscommunication about the patient instructions and follow-up appointments can lead to patient dissatisfaction and delays in discharge [14]. Because of the discharge planning program, physicians must instruct patients on post-discharge care precautions, medication, etc. They must also conduct telephone follow-up visits after patients have been discharged to understand patients’ actual status after discharge. Telephone calls to patients after discharge from the hospital are confirmed as an important part of care transitions [15].
In the past, patients were returned to the attending physician’s office for follow-up, and residents often ended their care of patients after discharge and knew nothing about the patients’ condition after discharge. Phone calls allow residents to know how patients are doing after discharge and to really understand the importance of discharge planning for patients. They become more aware of the importance of discharge planning, and the residents’ connection to patients is more comprehensive and uninterrupted. PGY residents also care more about quality of patient care.